Sarah Martinez was 52 when her hands started trembling. At first, she thought it was just stress from her demanding job as a teacher, but when the tremors persisted and walking became increasingly difficult, her doctor delivered devastating news: early-onset Parkinson's disease. Like millions of people worldwide facing neurological conditions, Sarah was told that while medications could help manage her symptoms, there was no cure and no way to stop the progression of her disease.
That was three years ago. Today, Sarah is participating in a groundbreaking clinical trial using stem cell therapy, and for the first time since her diagnosis, she has reason for hope. Her story represents a new chapter in treating neurological conditions that have long been considered incurable.
The human brain, with its 86 billion neurons connected by trillions of synapses, has always been considered the body's most complex and least regenerative organ. Unlike your skin, which replaces itself every few weeks, or your liver, which can regrow from just a quarter of its original size, the brain was thought to have very limited ability to repair itself once damaged. This belief made neurological conditions like Parkinson's disease, Alzheimer's disease, and stroke particularly devastating – once brain cells died, they were gone forever.
Stem cell therapy is changing that paradigm entirely. These remarkable treatments are showing that the brain may have far more capacity for healing and regeneration than we ever imagined, but it needs the right cellular tools to unlock that potential.
Understanding the Neurological Challenge
To appreciate why stem cell therapy represents such a breakthrough for neurological conditions, it's important to understand what makes these diseases so difficult to treat. Unlike conditions that affect organs with good regenerative capacity, neurological diseases attack the very cells that make us who we are – the neurons that control our movements, store our memories, and enable us to think.
Parkinson's disease specifically targets dopamine-producing neurons in a brain region called the substantia nigra. These neurons are crucial for controlling smooth, coordinated movement. As they die off, patients develop the characteristic symptoms of Parkinson's: tremors, rigidity, slow movement, and balance problems. Traditional treatments focus on replacing the missing dopamine with medications, but they don't address the underlying problem – the continued death of neurons.
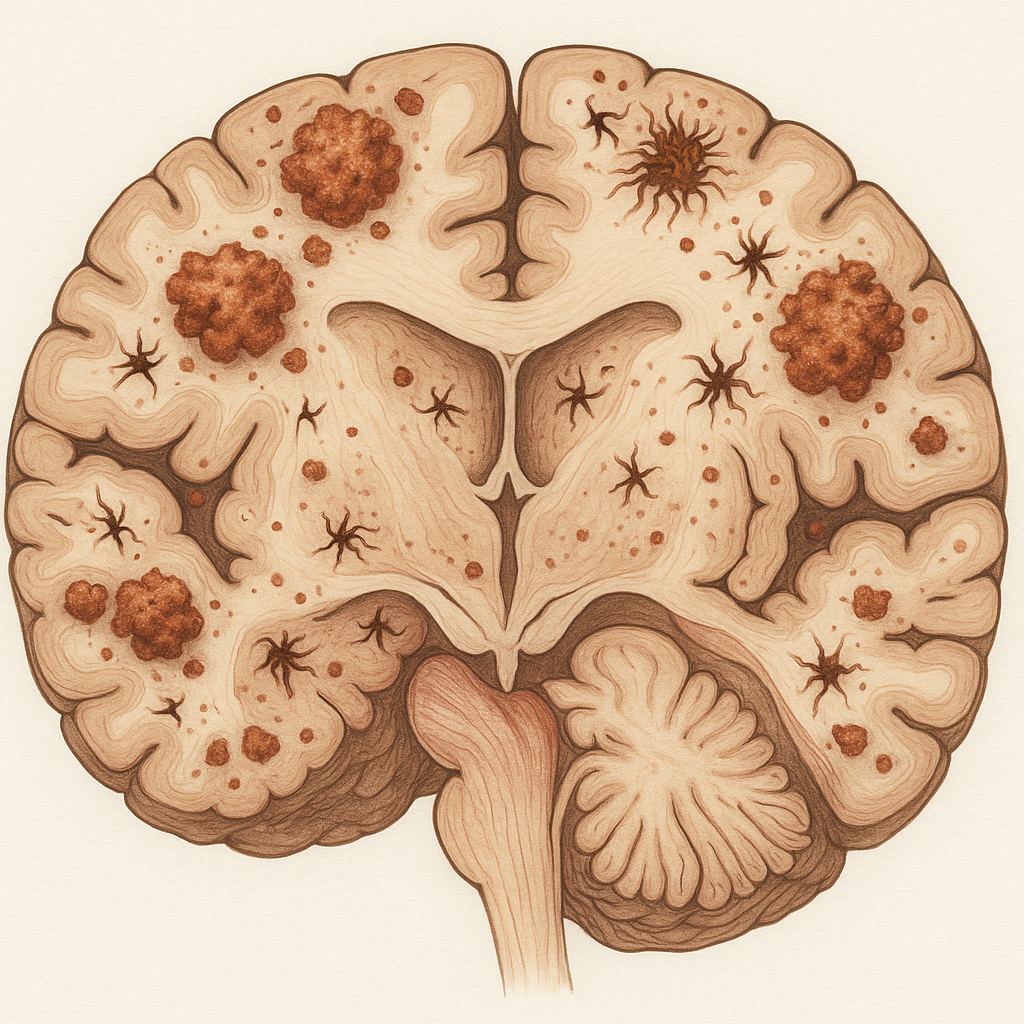
Alzheimer's disease follows a different but equally devastating pattern. This condition involves the accumulation of toxic proteins that damage and kill brain cells, particularly in areas responsible for memory and thinking. As neurons die and brain tissue shrinks, patients progressively lose their ability to remember, reason, and eventually care for themselves.
Stroke represents a third category of neurological damage. When blood flow to part of the brain is blocked or when a blood vessel ruptures, brain cells in the affected area die within minutes from lack of oxygen. The damage is often sudden and severe, leaving patients with paralysis, speech problems, or cognitive difficulties that traditional medicine has had limited ability to reverse.
What these conditions share is the death of irreplaceable brain cells. Until recently, medicine could only offer treatments to manage symptoms or slow progression – there was no way to actually replace the neurons that had been lost.
The Parkinson's Breakthrough: Growing New Dopamine Neurons
The field of neurological stem cell therapy has perhaps made its most dramatic advances in treating Parkinson's disease. The concept is elegantly simple: if Parkinson's is caused by the death of dopamine-producing neurons, why not replace them with new ones grown from stem cells?
This idea has been pursued for decades, but early attempts faced numerous challenges. Researchers tried transplanting dopamine neurons from fetal tissue, but the supply was extremely limited and the procedures raised ethical concerns. The neurons often didn't survive well after transplantation, and some patients developed troublesome side effects.
The development of induced pluripotent stem cells (iPSCs) changed everything. Scientists can now take ordinary skin cells from patients, reprogram them to become pluripotent stem cells, and then guide those stem cells to become dopamine-producing neurons that are genetically identical to the patient's own cells.
In 2024, researchers published remarkable results from clinical trials using this approach. Patients who received transplants of their own iPSC-derived dopamine neurons showed significant improvements in motor function, with some experiencing reductions in tremors and improvements in movement that were maintained for years after treatment.
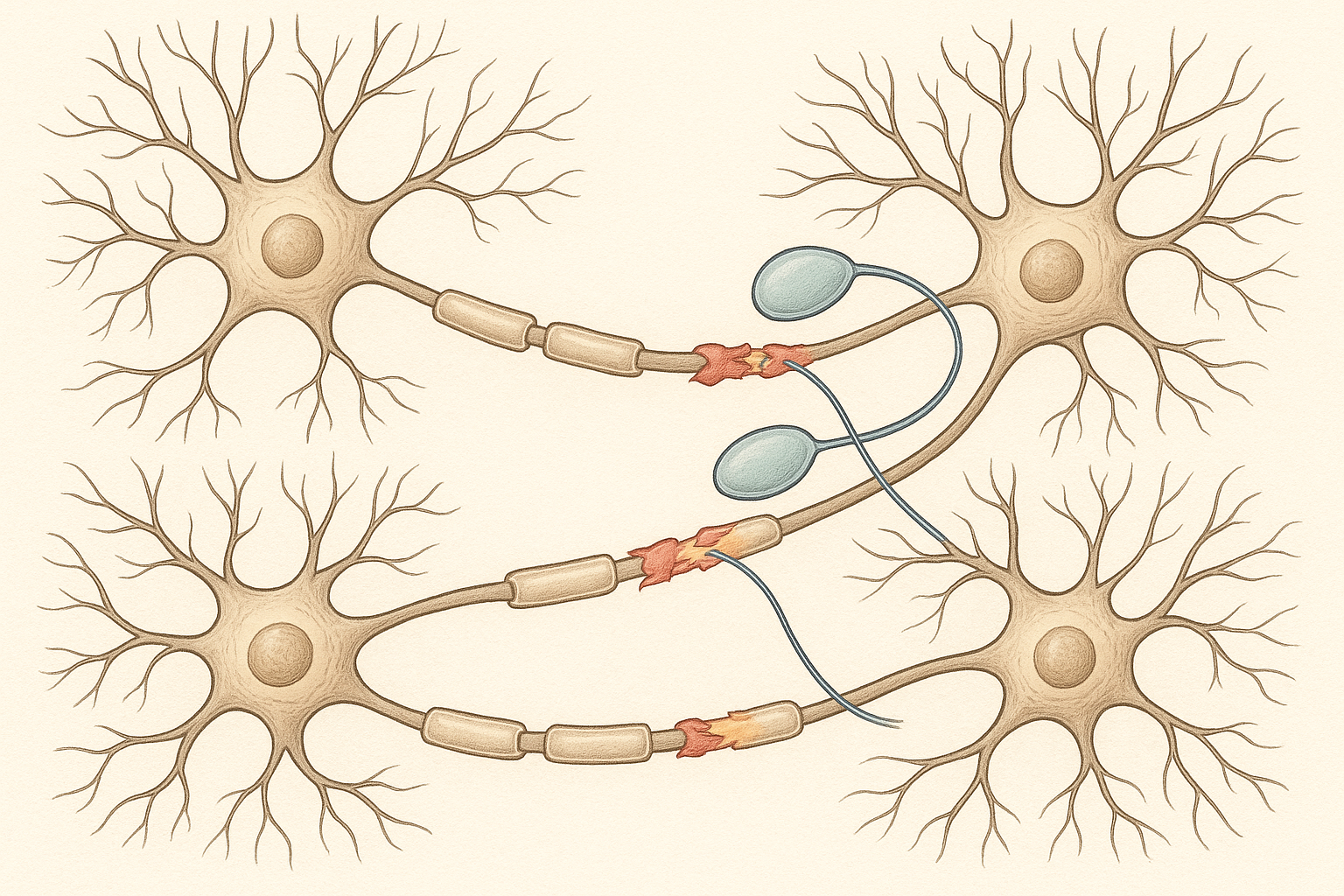
One of the most compelling aspects of these trials is how the transplanted neurons actually integrate with the patient's existing brain circuits. Using advanced brain imaging, researchers can see the new neurons forming connections and producing dopamine in the exact locations where it's needed. It's not just symptom management – it's actual restoration of brain function.
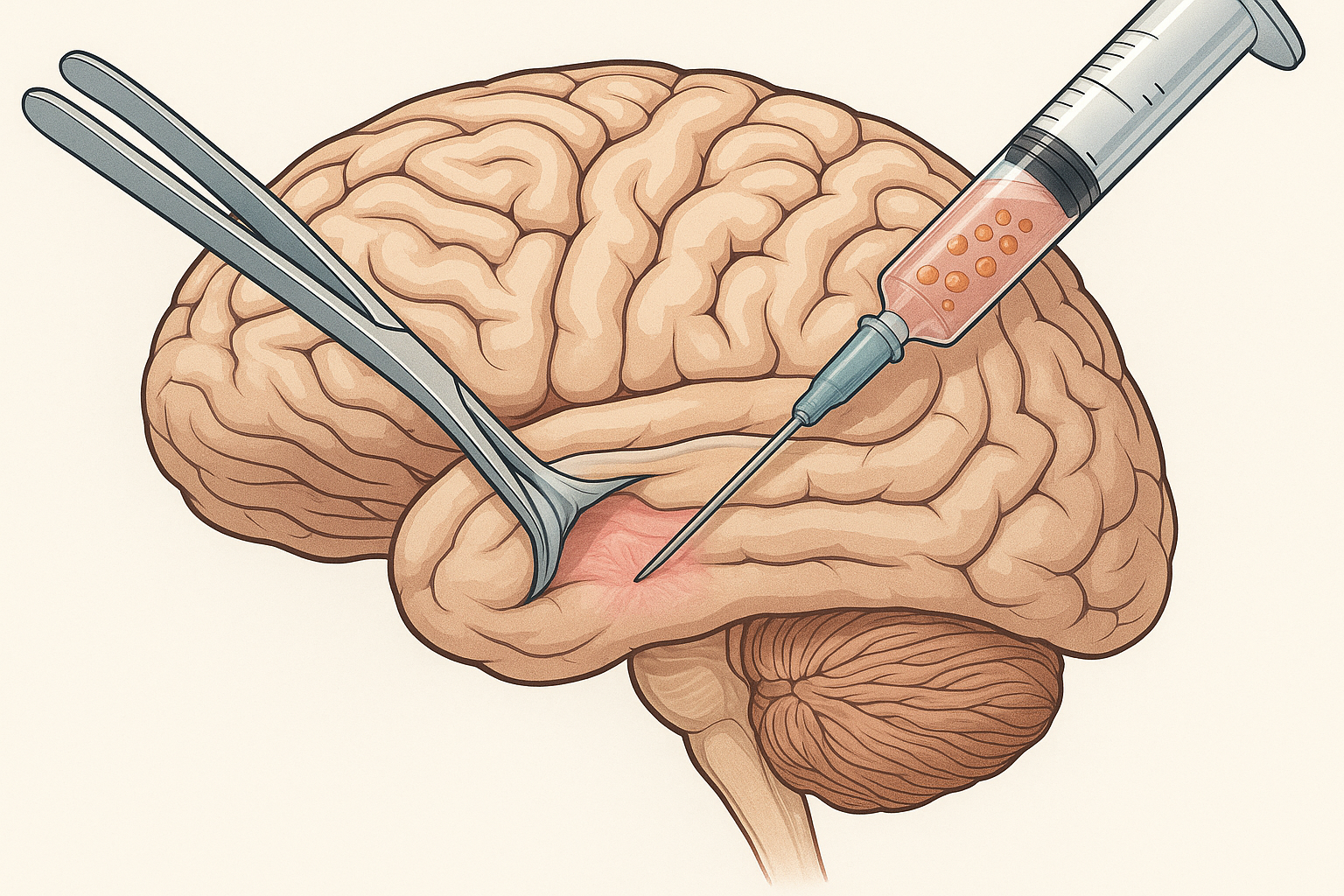
The procedure itself is remarkably sophisticated yet straightforward. Patients undergo stereotactic surgery, where surgeons use precise imaging guidance to inject the stem cell-derived neurons into specific locations in the brain. The entire procedure takes several hours, but patients typically go home within a few days.
Alzheimer's Disease: Attacking Multiple Targets
Treating Alzheimer's disease with stem cell therapy presents different challenges than Parkinson's. While Parkinson's primarily affects one type of neuron in a specific brain region, Alzheimer's causes widespread damage throughout the brain, affecting multiple types of neurons and disrupting complex networks of brain connections.
However, recent clinical trials are showing promising results using a multi-pronged approach. Rather than trying to replace all the lost neurons, researchers are focusing on using stem cells to:
First, clear out the toxic proteins that cause Alzheimer's. Certain types of stem cells can be engineered to produce enzymes that break down amyloid plaques and tau tangles – the protein deposits that accumulate in Alzheimer's patients' brains and contribute to neuron death.
Second, reduce inflammation in the brain. Alzheimer's involves chronic inflammation that accelerates brain damage. Some stem cell therapies use mesenchymal stem cells that have powerful anti-inflammatory properties, helping to create a more favorable environment for the brain's own repair processes.
Third, promote the survival and function of remaining neurons. Even in advanced Alzheimer's, many neurons are damaged but not yet dead. Stem cells can secrete growth factors and other supportive molecules that help these struggling neurons recover and function better.
Fourth, stimulate the brain's own regenerative processes. Recent research has shown that the adult brain continues to produce new neurons throughout life, particularly in areas involved in memory formation. Stem cell therapies can enhance this natural neurogenesis, potentially helping to compensate for neurons lost to the disease.
Early results from clinical trials using this comprehensive approach have been encouraging. While stem cell therapy hasn't cured Alzheimer's, patients have shown improvements in cognitive testing, daily functioning, and quality of life measures. Perhaps most importantly, some patients have shown slowing of disease progression, giving them and their families precious additional time.
Stroke Recovery: Rewiring the Brain
Stroke presents unique opportunities and challenges for stem cell therapy. Unlike the gradual progression of Parkinson's or Alzheimer's, stroke damage happens suddenly, often affecting large areas of the brain. However, this also means that the specific areas needing repair are clearly defined, making it easier to target stem cell treatments precisely.

The brain's response to stroke involves several phases, and stem cell therapy can potentially help during multiple stages of recovery. In the acute phase immediately after stroke, the focus is on limiting damage and preventing further cell death. In the chronic phase, which can last months or years, the focus shifts to promoting recovery and rebuilding function.
Recent clinical trials have tested stem cell therapy in both acute and chronic stroke patients, with remarkable results in both groups. For acute stroke patients, stem cells appear to help limit the spread of damage and protect neurons that are injured but not yet dead. For chronic stroke patients – some treated years after their initial stroke – stem cells have helped promote recovery that was previously thought impossible.
The mechanisms by which stem cells help stroke recovery are fascinating and complex. Some of the transplanted stem cells directly replace dead neurons, but many appear to work by supporting the brain's natural healing processes. They secrete growth factors that encourage surviving neurons to form new connections, promote the growth of new blood vessels to improve blood flow to damaged areas, and reduce inflammation that can impede recovery.
One of the most exciting discoveries is that stem cell therapy can help the brain reorganize itself after stroke. The brain has remarkable plasticity – the ability to rewire itself and have healthy areas take over functions from damaged regions. Stem cells appear to enhance this plasticity, helping patients recover functions that seemed permanently lost.
Different Types of Stem Cells, Different Approaches
Not all stem cell therapies for neurological conditions use the same types of cells, and understanding these differences helps explain why treatments vary between conditions and patients.
Embryonic stem cell-derived therapies use cells that have been guided to become specific types of neurons before transplantation. This approach is particularly useful for conditions like Parkinson's, where the goal is to replace specific types of neurons that have been lost.
Induced pluripotent stem cell therapies use the patient's own cells that have been reprogrammed and then differentiated into the needed cell types. This approach eliminates concerns about immune rejection and provides a potentially unlimited supply of patient-specific cells.
Mesenchymal stem cell therapies use adult stem cells that are primarily valuable for their ability to secrete beneficial substances rather than to become neurons themselves. These treatments are often used for their anti-inflammatory and neuroprotective effects.
Neural stem cell therapies use stem cells that are already committed to becoming brain cells. These cells can differentiate into neurons and the supporting cells that help neurons function, making them particularly useful for conditions that affect multiple types of brain cells.
Each approach has advantages and limitations. Embryonic stem cell-derived therapies offer the most potent cells but require careful immune management. iPSC therapies avoid immune problems but require more time to prepare personalized treatments. Mesenchymal stem cells are easier to obtain and use but may have more limited effects. Neural stem cells are naturally suited for brain repair but can be difficult to obtain in sufficient quantities.
The Treatment Experience: What Patients Can Expect
For patients considering neurological stem cell therapy, understanding what the treatment experience involves can help with decision-making and preparation. While specific procedures vary depending on the condition being treated and the type of stem cells used, there are common elements to most neurological stem cell treatments.
The process typically begins with extensive evaluation to determine if a patient is a good candidate for treatment. This includes detailed neurological examinations, brain imaging studies, and often neuropsychological testing to establish baseline function. Patients may also undergo medical tests to ensure they're healthy enough for the procedure.
For treatments using the patient's own cells, the next step is cell collection. This might involve a simple blood draw, a small skin biopsy, or a bone marrow aspiration, depending on the cell source. The collected cells are then sent to specialized laboratories where they're processed and, if necessary, reprogrammed and differentiated into the desired cell types.
The actual treatment delivery varies significantly between different approaches. Some therapies involve direct injection into the brain through small holes drilled in the skull – a procedure called stereotactic injection. While this sounds intimidating, it's performed under careful anesthesia with precise computer guidance, and most patients tolerate it well.
Other therapies are delivered through less invasive routes. Some stem cells can be given intravenously and will migrate to the brain on their own. Others can be delivered through the spinal fluid via lumbar puncture. Some experimental approaches even deliver stem cells through the nose, taking advantage of direct pathways from the nasal cavity to the brain.
Recovery from the procedure itself is usually straightforward, but seeing benefits from the treatment takes time. Unlike conventional medications that might work within hours or days, stem cell therapies often take weeks or months to show their full effects. This is because the stem cells need time to integrate, differentiate, and begin supporting brain repair processes.
Global Perspectives: Where Treatments Are Available
The availability of neurological stem cell therapies varies significantly around the world, reflecting differences in regulatory approaches, healthcare systems, and research infrastructure. Understanding this global landscape can help patients navigate their options.
The United States has some of the most rigorous regulatory oversight of stem cell therapies, which has both benefits and drawbacks. The thorough FDA approval process helps ensure safety and efficacy, but it also means that many promising treatments remain in clinical trials and aren't yet available to most patients. However, US patients may be able to access experimental treatments through clinical trials at major medical centers.
Europe has a somewhat more flexible regulatory environment, with some countries allowing conditional approval of stem cell therapies based on preliminary evidence while longer-term studies continue. The European Medicines Agency coordinates oversight across member countries, but individual nations can make their own decisions about treatment availability.
Japan has emerged as a leader in neurological stem cell therapy, particularly for conditions like Parkinson's disease and stroke. The country's regenerative medicine legislation allows for conditional approval of treatments with promising preliminary results, meaning patients can access some therapies that are still in clinical trials elsewhere.
South Korea, despite past controversies in stem cell research, has developed robust regulatory frameworks and is conducting important clinical trials. The country has particular expertise in iPSC technologies and is testing several neurological applications.
China has significant stem cell research capabilities and has conducted large clinical trials, though regulatory oversight has historically been less stringent than in other countries. Recent changes are increasing oversight while still allowing relatively broad access to experimental treatments.
Several other countries, including Israel, Australia, and Canada, have active neurological stem cell research programs and may offer access to treatments through clinical trials or compassionate use programs.
Success Stories and Realistic Expectations
While the potential of neurological stem cell therapy is enormous, it's important to balance hope with realistic expectations. The field has produced genuine success stories, but it has also seen disappointments and setbacks.
David Chen, a 68-year-old engineer, participated in a stem cell trial for Parkinson's disease and experienced significant improvement in his symptoms. Two years after treatment, his tremors had diminished substantially, his movement was much smoother, and he was able to reduce his Parkinson's medications. Brain scans showed that the transplanted cells were functioning and producing dopamine.
Maria Rodriguez received stem cell therapy six months after a stroke left her unable to speak or move her right arm. Over the following year, she gradually regained both speech and arm function. While she hasn't returned to her pre-stroke baseline, the improvements have allowed her to live independently and return to many activities she enjoys.
However, not all patients see such dramatic results. Some experience modest improvements, others see temporary benefits that fade over time, and some don't improve at all. The factors that determine who will respond well to treatment are still being studied, making it difficult to predict outcomes for individual patients.
Age appears to be a factor, with younger patients often showing better responses. The severity and duration of the condition also matter – patients with earlier-stage disease or more recent injuries often respond better than those with advanced, long-standing conditions. Individual genetic factors, overall health status, and even lifestyle factors like exercise and diet may influence outcomes.
Safety Considerations and Risk Management
Like any medical intervention, neurological stem cell therapy carries risks that must be carefully weighed against potential benefits. Understanding these risks helps patients make informed decisions about treatment options.
The most serious risk is related to the brain surgery often required to deliver stem cells. While stereotactic procedures are generally safe, they do carry small risks of bleeding, infection, or other complications. Modern imaging guidance and surgical techniques have made these procedures much safer than in the past, but they're not risk-free.
There are also risks specific to the stem cells themselves. Undifferentiated stem cells can potentially form tumors, though this risk appears to be very low with properly prepared and tested cell preparations. Some patients may experience immune reactions to transplanted cells, even when using their own cells that have been manipulated in the laboratory.
Neurological side effects are another concern. Because stem cell therapy can affect brain function, patients might experience changes in movement, sensation, thinking, or behavior. Most of these effects are mild and temporary, but they can occasionally be significant.
Long-term risks are still being studied. Because neurological stem cell therapy is relatively new, we don't yet know what might happen to patients 10, 20, or 30 years after treatment. Long-term follow-up studies are ongoing to monitor for any delayed effects.
To minimize risks, patients should only consider treatment from reputable medical centers with proper regulatory oversight and extensive experience in stem cell therapy. Treatment should always be part of a comprehensive care plan that includes appropriate monitoring and follow-up.
The Economics of Hope: Costs and Insurance
The cost of neurological stem cell therapy can be substantial, and insurance coverage is often limited. Understanding the financial aspects is crucial for patients considering these treatments.
Experimental treatments provided through clinical trials are typically free to patients, with research sponsors covering all costs. This makes clinical trials an attractive option for patients who qualify, though not everyone meets the strict inclusion criteria.
For commercially available treatments, costs can range from tens of thousands to over $100,000, depending on the specific therapy and location. These costs reflect the complex manufacturing processes required to prepare stem cells, the specialized medical expertise needed to deliver treatments safely, and the extensive monitoring required.
Insurance coverage for neurological stem cell therapy is currently limited. Most treatments are still considered experimental by insurance companies, meaning patients must pay out of pocket. However, this is beginning to change as some therapies demonstrate clear benefits in clinical trials and receive regulatory approval.
Some medical centers offer financing options or payment plans to help make treatments more accessible. Patient advocacy organizations sometimes provide grants or other financial assistance for specific conditions. It's worth exploring all options with treatment centers and insurance providers, as coverage policies are evolving rapidly.
The Role of Rehabilitation and Supportive Care
Stem cell therapy doesn't work in isolation – it's most effective when combined with comprehensive rehabilitation and supportive care. Understanding this integrated approach is crucial for maximizing treatment benefits.
Physical therapy plays a vital role in neurological stem cell therapy outcomes. For stroke patients, intensive physical therapy helps the brain learn to use newly formed neural connections. For Parkinson's patients, exercise and movement therapy can enhance the benefits of stem cell treatments and may even help transplanted cells integrate better.
Occupational therapy helps patients regain practical skills needed for daily living. Speech therapy is crucial for patients with language or swallowing problems. Cognitive rehabilitation can help patients with thinking and memory difficulties make the most of any improvements from stem cell therapy.
Nutritional support, stress management, and adequate sleep all play important roles in brain health and may influence stem cell therapy outcomes. Some treatment centers provide comprehensive programs that address all these factors, while others work with patients to coordinate care with local providers.
The timing and intensity of rehabilitation may need to be adjusted based on stem cell therapy. Some patients may benefit from intensive therapy immediately after treatment, while others might need to start more gradually as the stem cells begin to take effect.
Looking to the Future: Next-Generation Treatments
The field of neurological stem cell therapy is advancing rapidly, with new approaches and improvements to existing treatments being developed constantly. Understanding these future directions provides insight into what may become available in the coming years.
Gene editing technologies like CRISPR are being combined with stem cell therapy to create more powerful treatments. Scientists can now modify stem cells to make them more effective at repairing brain damage or to give them new capabilities, such as producing therapeutic proteins.
Bioengineering approaches are creating more sophisticated ways to deliver stem cells to the brain. Researchers are developing biodegradable scaffolds that can support stem cell growth and guide their development into organized tissue structures. Others are creating microspheres that can deliver stem cells along with growth factors and other beneficial substances.
Artificial intelligence is being used to optimize stem cell therapies, helping to predict which patients will respond best to treatment and to personalize therapy protocols. Machine learning algorithms can analyze complex patterns in brain imaging, genetic data, and clinical information to guide treatment decisions.
Combination therapies that use multiple types of stem cells or combine stem cells with other treatments are showing promise. For example, researchers are testing combinations of neural stem cells with mesenchymal stem cells, or stem cell therapy combined with growth factors or pharmacological agents.
Making the Decision: Is Stem Cell Therapy Right for You?
Deciding whether to pursue neurological stem cell therapy is a complex decision that should involve careful consideration of many factors and consultation with qualified medical professionals.
The first consideration is whether you're a candidate for treatment. This depends on your specific condition, its severity and progression, your overall health status, and other factors. Most treatment centers have specific criteria for patient selection, and not everyone will qualify.
The potential benefits must be weighed against the risks and costs. While some patients experience dramatic improvements, others see modest benefits or no improvement at all. The likelihood of benefit varies by condition, with some neurological disorders showing more consistent responses to stem cell therapy than others.
Your personal circumstances and values also matter. Some patients are willing to accept significant risks and costs for even a small chance of improvement, while others prefer to wait for more established treatments. Consider your quality of life goals, your support system, and your financial situation.
It's also important to consider the time commitment involved. Neurological stem cell therapy often requires multiple medical center visits, extended evaluation periods, and long-term follow-up. Some patients need to travel significant distances for treatment, which can add logistical complexity and cost.
Finally, consider your alternatives. Are there other treatments available for your condition that might be more appropriate? Could participating in a clinical trial provide access to cutting-edge treatments while contributing to research? Would focusing on rehabilitation and supportive care be more beneficial at this time?
The decision should be made in consultation with neurologists or other specialists who understand both your specific condition and the current state of stem cell therapy. Seek multiple opinions if necessary, and don't rush the decision-making process.
The Broader Impact: Changing How We Think About Brain Disease
Neurological stem cell therapy is doing more than just providing new treatments – it's fundamentally changing how we think about brain disease and recovery. For decades, the prevailing view was that neurological conditions were largely irreversible and that the best medicine could do was manage symptoms and slow progression.
Stem cell therapy has challenged this paradigm by demonstrating that the brain has far more capacity for repair and regeneration than previously believed. This shift in understanding is influencing all aspects of neurological care, from how diseases are studied to how patients are counseled about their prognosis.
The success of stem cell therapy is also spurring innovation in other areas of neurological treatment. If the brain can be coaxed to repair itself with the right cellular support, what other interventions might promote healing? This question is driving research into new drugs, medical devices, and rehabilitation approaches.
Perhaps most importantly, stem cell therapy is providing hope to patients and families facing devastating neurological conditions. Even for patients who don't yet have access to these treatments, knowing that research is actively working toward cures rather than just symptom management can provide psychological benefits and motivation to maintain health while waiting for treatments to become available.
The field still faces significant challenges. Not all patients respond to treatment, the mechanisms of action aren't fully understood, and long-term safety data is still being collected. Manufacturing high-quality cell products at scale remains expensive and complex. Regulatory pathways for approval need to balance innovation with safety.
However, the progress made in just the past few years has been remarkable. Treatments that seemed like science fiction a decade ago are now helping real patients recover from conditions that were considered incurable. As research continues and technologies improve, the potential for stem cell therapy to transform neurological medicine becomes increasingly clear.
For patients like Sarah Martinez, who are living with neurological conditions today, stem cell therapy represents more than just a medical treatment – it represents the possibility that their conditions may not define the rest of their lives. While not every patient will experience dramatic recovery, the field has moved from managing decline to actively promoting healing.
The future of neurological stem cell therapy looks bright, with new treatments entering clinical trials regularly and existing therapies being refined and improved. As our understanding of the brain's regenerative capacity grows and our ability to harness stem cells becomes more sophisticated, we may be entering an era where neurological conditions that have plagued humanity for centuries finally become treatable, and perhaps even curable.
This transformation won't happen overnight, and there will undoubtedly be setbacks and disappointments along the way. But for the first time in history, we have scientific tools that can actually repair damaged brain tissue and restore lost function. That represents a fundamental shift in the fight against neurological disease, and it offers genuine hope to millions of patients and families worldwide.


